65 year old male with tremors and urinary incontinence
This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from an available global online community of experts to solve those patients clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
Following is the view of my case :
Date of admission : 12/11/2022
Chief complaints :
C/O Tremors since 5 years,
Giddiness since 2 months
Uncontrolled urination since 2 months
Slurring of speech since 3 months
History of presenting illness:
Patient was apparently asymptomatic 5 years ago then he developed tremors in upper limbs which was insidious in onset and gradually progressive and involved lower limbs,3 months back his speech got slurred, drooling of saliva started,since 2 months patient was unable to control micturition and he started to felt giddiness and falls suddenly while walking and he is complaining of constipation since 2 months
No H/O Fever, Vomitings, burning micturition,chills, SOB
Past history:
He is a K/C/O Parkinson's disease and he is using Syndopa 125 mg and trihexiphenidyl 2mg since 3 years
No history of similar complaints in the past
N/K/C/O DM,Htn,Tb,Asthma, epilepsy,CAD,
Thyroid disorders
Family History:
Not Significant
Personal History:
Diet - mixed
Appetite - normal
sleep - adequate
Bowel and Bladder movements- irregular, constipation and urinary incontinence is seen
Addictions - no
No known allergies
Drug history :
No significant drug history
General examination:
Patient is conscious ,coherent ,cooperative and was well oriented to time ,place and person
at the time of examination
He is examined in a well lit room, with consent taken.
He is moderately built and moderatly nourished.
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
lymphadenopathy - absent
Pedal edema - absent
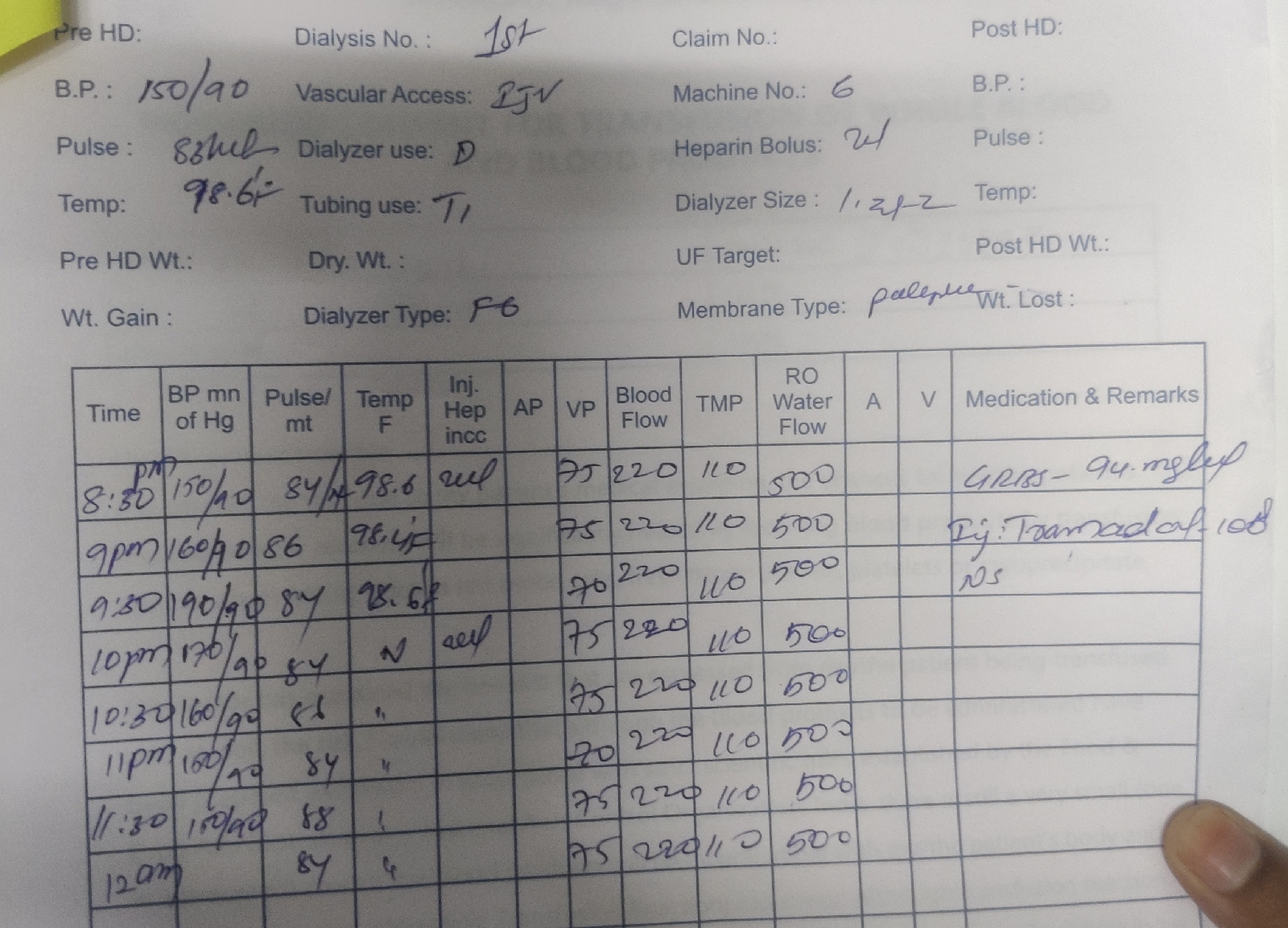
Vitals : on the day of admission (12/11/2022)
Temperature - afebrile
Pulse rate - 82 bpm
Respiratory rate - 16 cpm
Blood pressure - 120/80 mmHg
SpO2 - 99% on Room air
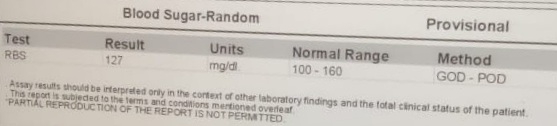
GRBS - 127 mg/dl
Postural hypotension not present:
- Supine BP - 120/70mmHg & On Standing 120/80mmHg
Systemic examination:
CVS : S1 and S2 heart sounds heard
NO murmurs and thrills
RESPIRATORY SYSTEM : Bilateral air entry present position of trachea - central
Vesicular breathsounds heard
CNS : mask like expression less face is seen
Festinant gait present
Able to do finger nose test,knee heal test,no dysdiadokokinesia,
Not able to walk in a straight line
ABDOMEN :
Soft
On deep palpation -non TENDER no palpable masses
Bowel sounds heard
NO organomegaly
Investigations:
On 12/11/2022:
On 13/11/2022:
HEMOGRAM:
SERUM CREATININE:
SERUM ELECTROLYTES:
SERUM CALCIUM:
COMPLETE URINE EXAMINATION:
BLOOD SUGAR-RANDOM:
BLOOD UREA:
LIVER FUNCTION TEST:
Anti HCV Antibodies-RAPID:
HBsAg-RAPID:
HIV1/2 RAPID :
X-ray :
Ultrasound Report:
ECG Report:
On 14/11/2022:
Diagnosis:
Parkinson's disease
Treatment:
1)Tab.Syndopa 125 mg PO/TD
2)Tab.Trihexyphenidyl 2 mg PO/BD
3)Inj. Optineuron 1amp in 500ml NS IV/OD



















Comments
Post a Comment