A 27 year old male patient came with abdominal pain
This is online E-blog, to discuss our patient de-identified health data shared after taking her guardian's signed informed consent.



Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-blog also reflects my patient's centred online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case...
CASE:
27 year old male patient who is a resident of vemanapalli and electrician by occupation came to OPD with chief complaints of abdominal pain since 3 months(November 2021
History of presenting illness:
Patient was apparently asymptomatic 4 months back then he had vomitings which were non projectile ,bilious,green in colour, contents were food material he had ate,vomitings come immediately after eating food
Then he went to a government hospital in Vijayawada and symptomatic treatment is given but vomitings are not subsided
He went to a another private hospital in Vijayawada there they inserted a tube through his mouth and removed green coloured liquid which was almost a litre in amount,from then the vomitings are subsided and they treated him as pancreatitis case
Then he developed abdominal pain in the middle of November 2021 which was sudden in onset, intermittent in nature , squeezing type of pain,which was increased on taking the food very severly persists for 2 to 3 hours after taking medication it relieves and pain is referred to back and it is more around the left hypochondrium and epigastrium and sometimes pain gets relieved by resting in between the meal timings
Patient was referred to a Contrast enhanced CT scan of abdomen in the same private hospital,after taking the contrast he had severe vomiting once and from the CT results patient was declared as having pancreatitis with pseudocyst
Patient was discharged and he had symptom free interval for 7 to 10 days and he again developed abdominal pain which is intermittent and relieved by taking medication
He had covid infection in January 2022 and he took treatment in home isolation
He reffered to our hospital and he came to our hospital on 7-2-2022
Past History:
Not a known case of Diabetes, hypertension,asthma, tuberculosis,CHD,thyroid disorders
Family History:
Not significant
Personal History:
Diet-mixed
▪ Appetite-increased
▪Bowel movements-Regular
▪Bladder movements-Regular
▪Sleep -inadequate
▪Habits- he was alcoholic and not a smoker from last 4 years
daily he drinks alcohol of 500 to 600 ml till October ending
GENERAL EXAMINATION
▪Patient is conscious , coherent and cooperative and well oriented to time place
and person, moderately built and moderately nourished
- Pallor- absent
-Icterus-absent
-Cyanosis-absent
-Clubbing-absent
-Lymphadenopathy-absent
-Edema-absent
ON EXAMINATION :
*Patient is conscious, coherent, cooperative.
* Pallor , Icterus,Clubbing, Cyanosis , Koilonychia, Edema and lymphadenopathy are absent
VITALS
Temp- Afebrile
Bp-100/80 mm hg
Pr- 84bpm
Rr-16cpm
Spo2- 99% on RA
Grbs : 102
SYSTEMIC EXAMINATION :
CVS -S1 S2 +; No Murmurs.
PER ABDOMEN -
1)Tenderness present in epigastric region and left hypochondrium
2)Rigidity present in the epigastric region and left hypochondrium
3)No gaurding
4)Bowel sounds present
CNS:- NAD
INVESTIGATIONS :-
#HEMOGRAM -
HB 10.5 GM/DL
TLC #10,500
N/L/E/M/B. #135/20/#40/05/00
PCV #32.5
MCV # 82.7
MCHC 32.6
RBC. #3.93
PLT. 5.5
CUE :-
ALBUMIN. NIL
BILE SALTS AND PIGMENTS NIL
PUS CELLS NIL
LFT :-
TB 0.48 MG/DL
DB 0.17 MG/DL
SGOT 13 IU/L
SGPT. 14 IU/L
ALP. # 291 IU/L
Tp. # 5.9 gm/dl
albumin. #2.92 gm/dl
A/G RATIO. 0.98
SERUM AMYLASE. 292
SEROLGY. NEGATIVE
CRP POSITIVE 2.4 MG/DL
USG:
CECT:
PROVISIONAL DIAGNOSIS:-
CHRONIC PANCREATITIS WITH PSEUDOCYST .
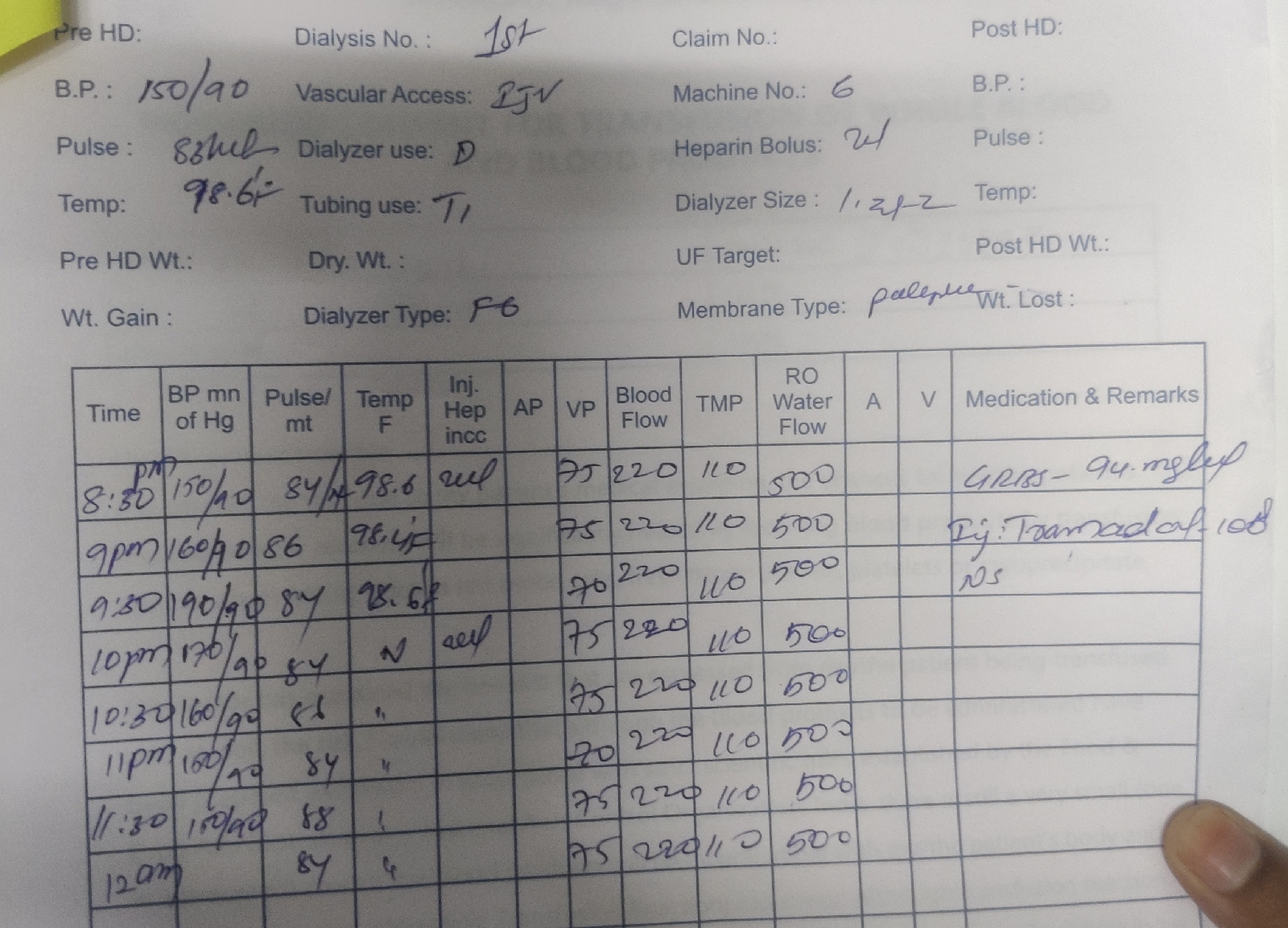
TREATMENT:-
1) IVF NS /RL @75 ml / hr
2) Inj Tramadol 100 ml IV /TID
3) Inj pantop 40 mg iv/ OD
4 ) Inj zofer 4 mg iv/sos.
5)Syrup. Cremaffin plus 15/ml/po.
Progress Notes:
Patient was sent for a gastroenterologist opinion and asked for endoscopy to be done
But endoscopy didn't done and advised for a surgical removal of pseudocyst


Comments
Post a Comment