70 year old female with fever and SOB
This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from an available global online community of experts to solve those patients clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
Following is the view of my case :
Date of admission : 30/10/2022
Chief complaints :fever since 20 days
Shortness of breath since 1day
History of presenting illness:
Patient was apparently asymptomatic 20 days back then she developed fever which was high grade and intermittent type,associated with generalized body weakness,chills, she went to a rmp near by and took some medication which relieved the fever for 2 days and again fever get started she went to another hospital in miryalaguda where she was diagnosed with Dengue and treated but she developed pain abdomen from 3 days and SOB since 1day for which she underwent an USG and diagnosed as ascites and was referred to our hospital She was complaining about difficulty in swallowing since 7 days
Past history:
Not a known case of DM,HTN,TB,CAD AND CVA,ASTHMA , EPILEPSY
FAMILY HISTORY:
NOT significant
Personal History:
Diet-mixed
Appetite-reduced
Bowel and Bladder movements- bowels movements reduced
Addictions:no
Allergies:no
Drug history:not significant
General examination :
Patient is conscious ,coherent ,cooperative and was well oriented to time ,place and person
at the time of examination
She is examined in a well lit room, with consent taken.
SHe is moderately built and moderatly nourished.
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
lymphadenopathy - absent
Pedal edema - absent
Vitals : on the day of admission :30/10/2022
Temperature - afebrile
Pulse rate - 82 bpm
Respiratory rate - 24 cpm
Blood pressure - 110/90 mmHg
SpO2 - 94% on Room air
GRBS - 92mg/dl
Systemic examination:
CVS:S1,S2 heard
RS:BAE present,NVBS heard
CNS:intact
Per abdomen: soft ,tender,no organomegaly detected
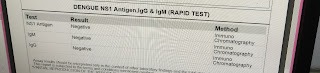
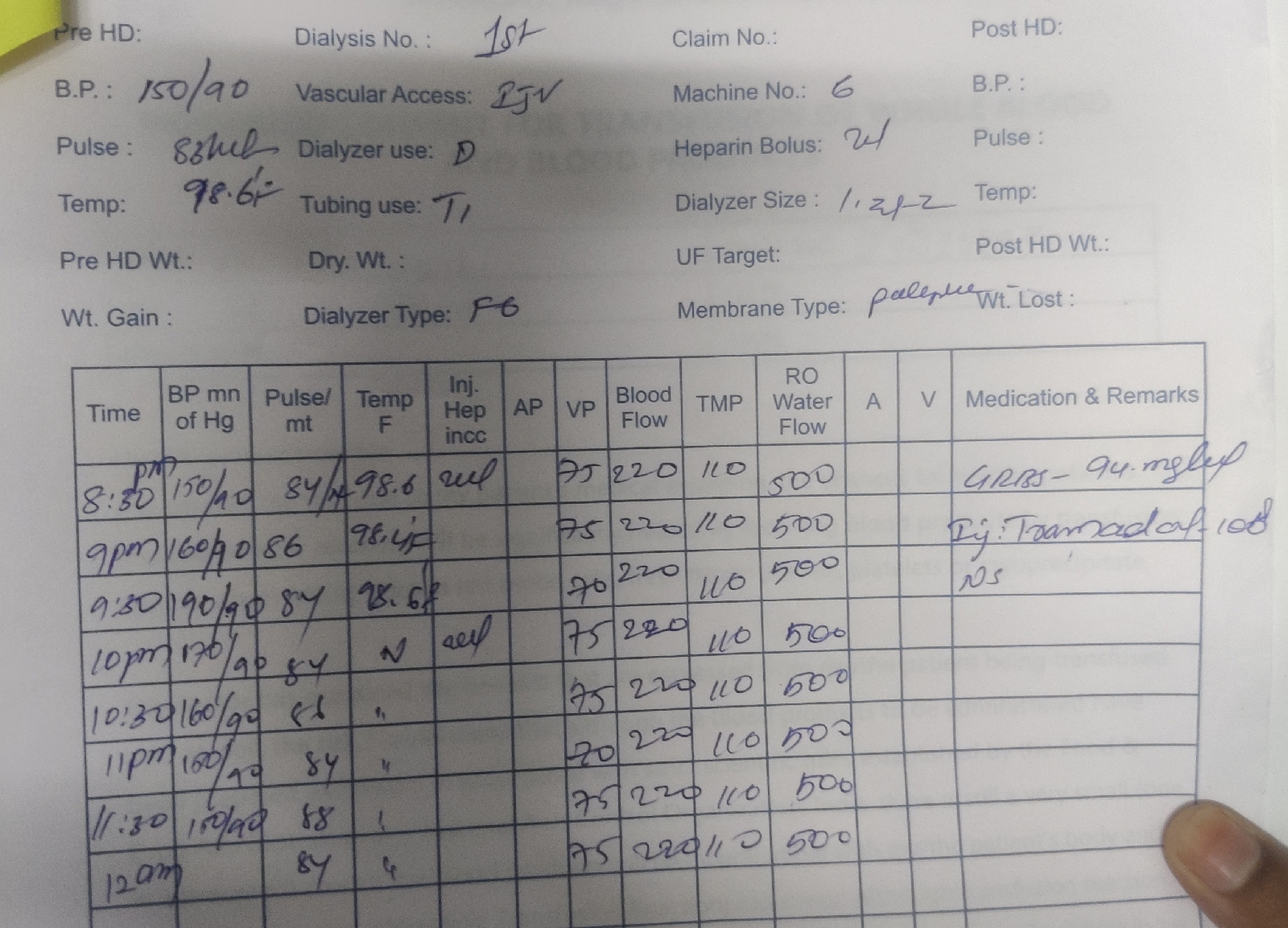
Investigations:
On 31/10/2022
On 31/10/22:
On 01/11/2022:
2/11/22:
Diagnosis:
Dengue with polyserositis
Treatment:
1)IV FLUIDS 2*NS,1*RL@100ml/hr
2)Tab PCM 650 mg PO TID
3)Tab Pan 40 mg PO OD
4) Temperature monitoring 4th hourly
5) Vitals monitoring 4 th hourly
6)Chlorexidine gargles in water 4times/day































Comments
Post a Comment