17 year old female with Fever Vomitings,SOB
This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from an available global online community of experts to solve those patients clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
Following is the view of my case :
Date of admission : 05/11/2022
Chief complaints :
C/O Fever,SOB, VOMITINGS, SINCE YESTERDAY MORNING
HOPI:
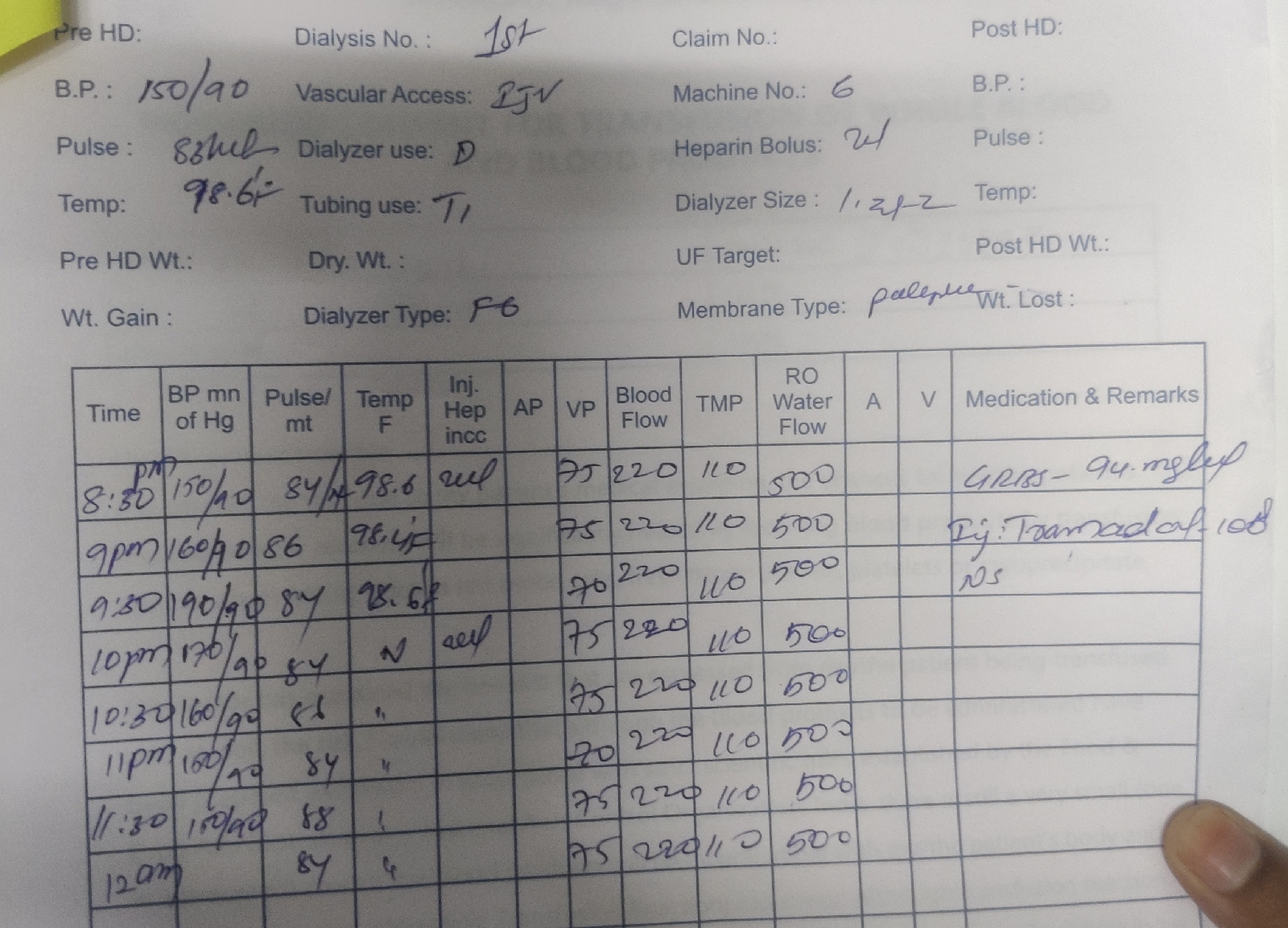
17 YEAR OLD FEMALE WAS APPARENTLY ALRIGHT TILL YESTERDAY MORNING THEN SHE HAD C/O FEVER WHICH WAS LOW GRADE IN NATURE FOLLOWED BY WHICH SHE SKIPPED HER MEAL AND INSULIN DOSE THEN SHE HAD C/O VOMITINGS WHICH WAS NON BILIOUS/NON PROJECTILE CONTAINING FOOD PARTICLES (8-10 EPISODES)&ALSO SHE HAD COMPLAINTS OF SOB AFTER WHICH,GRBS WAS SHOWN 550MG/DL &WAS GIVEN INSULIN DOSE THEN SHE WAS TAKEN TO LOCAL DOCTOR FROM WHERE SHE WAS REFFERRED TO HIGHER CENTER
PAST HISTORY:
K/C/O DM SINCE 7 YEARS AND IS ON INSULIN SINCE 3 YEARS
Family History:
Not Significant
Personal History:
Diet - mixed
Appetite - normal
sleep - adequate
Bowel and Bladder movements -passing black coloured stools
Addictions - no
No known allergies
Drug history :
No significant drug history
General examination :
Patient is conscious ,coherent ,cooperative and was well oriented to time ,place and person
at the time of examination
SHe is examined in a well lit room, with consent taken.
SHe is moderately built and moderatly nourished.
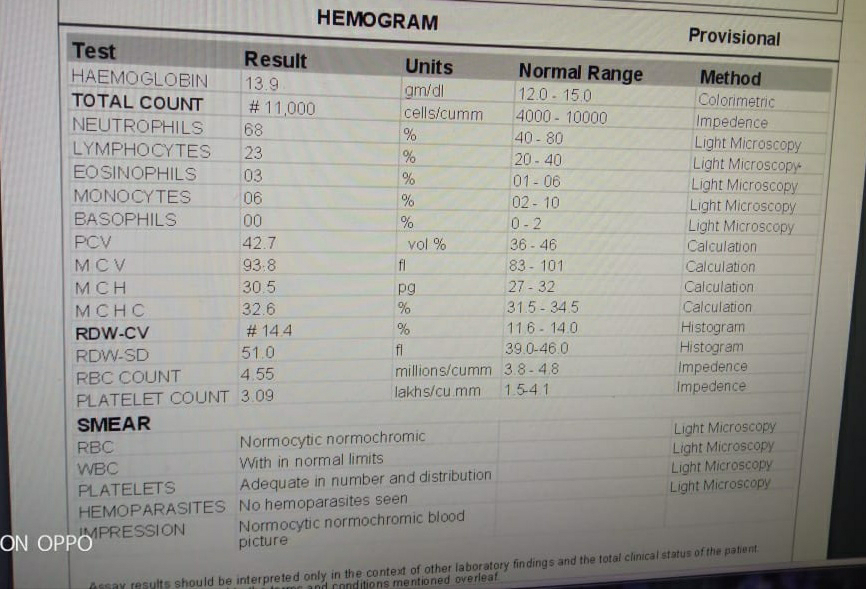
Pallor - present mild
Icterus - absent
Cyanosis - absent
Clubbing - absent
lymphadenopathy - absent
Pedal edema - absent
Vitals : on the day of admission (5/11/2022)
Temperature - afebrile
Pulse rate - 82 bpm
Respiratory rate - 18 cpm
Blood pressure - 110/70 mmHg
SpO2 - 99% on Room air
GRBS - 336 mg/dl
Systemic examination :
CVS : S1 and S2 heart sounds heard
NO murmurs and thrills
RESPIRATORY SYSTEM :
Bilateral air entry present position of trachea - central
Vesicular breathsounds heard
CNS : intact
ABDOMEN :
Soft
Non tender
No palpable masses
Bowel sounds heard
NO organomegaly
Investigations:
ABG :
pH - 7.19
pCO2 - 15.8
HCO3 - 5.8
pO2 - 120
CUE :
Her urine was positive for ketone bodies .
Sugar : +2
Albumin : trace
Pus cells : 3-4
Epithelial cells : 2-3
Diagnosis:
Diabetic ketoacidosis
Treatment:
1)IV fluids NS,RL,5%DEXTROSE@:100ml/hr
2) INJ pan 40mg IV OD
3)INJ ZOFER 4 MG IV BD
4) monitor vitals 4th hrly
5)INJ.MONOCEF 1GM IV BD
6) GRBS HRLY MONITORING
7)STRICT I O CHARTING
8)INJ.NEOMOL 1GM IV SOS(if temp >101)
9)Inj.Human Actrapid Insulin infusion@4ml/hr for 5 hrs (1ml insulin in 39 ml NS)
@2ml/hr for 5 hrs
10)If GRBS <250mg/dl-5%dextrose@100ml /hr: increased or decreased acc to GRBS
















Comments
Post a Comment